Oral and maxillofacial surgery is a very specific type of plastic surgery, but also one that’s becoming more popular as the world around us changes. What is oral and maxillofacial surgery? Oral and maxillofacial surgeons are dentists who have undergone additional training in the field of reconstructive surgery. They perform surgeries on patients with cleft palates, jaw injuries, facial fractures, and other issues that affect the mouth or jaw. They also perform cosmetic procedures like Botox injections and liposuction to help patients improve their appearance while maintaining function.
Oral surgeons work with patients from all walks of life: from kids with cleft palates to adults who have had an accident or injury that damaged their face or mouth. They are responsible for changing these lives for the better through reconstructive surgeries that aim to restore function as well as appearance to patients’ lives.
Read on to learn more about Is Oral And Maxillofacial Surgery Plastic Surgery, Types Of Sinus Surgery and Why Would I Get Sinus Surgery?

Is Oral And Maxillofacial Surgery Plastic Surgery
As an oral and maxillofacial surgeon (OMFS), you have developed a keen surgical aptitude that often includes ensuring sound cosmetic outcomes for your patients. If you find that you have a passion for the cosmetic aspect of your work, you may be considering making a career transition to the facial cosmetic surgery specialty.
The American Board of Facial Cosmetic Surgery (ABFCS) facilitates this pathway for interested OMFS with both single and dual degrees. If you are planning this career change, here are 8 key steps that our board-certified facial cosmetic surgeons recommend.
1. Find out if you are suited to the career change
Take time to consider whether you are suited to the career change. While your experience as an OMFS has largely addressed patients’ more straightforward medical needs, cosmetic surgeons’ work involves finding procedure(s) that address patients’ more nuanced requests and requirements. To succeed as a facial cosmetic surgeon, you should both be happy to work with patients’ individual preferences and have a natural aesthetic ability; your patients’ goals become your puzzle to creatively address with cosmetic procedures and treatments.
Reach out to practicing cosmetic surgeons, read about the specialty, and look for opportunities to shadow fellow doctors where possible. Our blog and webpage for surgeons offer insights, and the American Academy of Cosmetic Surgery (AACS) also offers many educational resources and conferences. Surgeons considering fellowship training may also consider reaching out to facial cosmetic fellowship directors, whose contact information is listed on our fellowship webpage.
2. Acquire training, i.e. through a cosmetic fellowship
There are three routes by which an oral and maxillofacial surgeon may specialize their practice and become a board-certified facial cosmetic surgeon: (1) the experience route, (2) the AACS-certified fellowship route (1-2 years), or (3) an equivalent non-AACS fellowship. Surgeons wishing to take the experience route will need to ensure they have extensive and proper documentation of cosmetic surgery cases; those who either prefer fellowship training or require it to gain experience may read more about fellowship training programs here.
3. Update malpractice insurance ahead of your fellowship
Whether you plan to begin offering cosmetic enhancements or are entering an AACS-certified facial cosmetic fellowship, update your malpractice insurance to reflect your change in practice. Cosmetic surgery fellows are also required to obtain an unrestricted medical license in the state where the fellowship is offered. (Fellowships are offered at cosmetic practices across the country).
4. Pass board certification
After you have successfully completed a fellowship or collected evidence of proficiency in facial cosmetic surgery, as well as met other requirements, you may petition the American Board of Facial Cosmetic Surgery (ABFCS) for board certification. Both single- and dual-degree oral and maxillofacial surgeons are eligible. Review requirements and learn how to apply here.

5. Be sure your before-and-after photo setup is up to cosmetic medicine standards
More so than any other specialty, facial cosmetic surgeons rely on before and after photos of patients as a critical tool. You will use before and after photos to demonstrate your surgical ability to patients and to communicate with them about their desired results in consultations. You will also want to include some before and after photos (with patient consent) in your marketing materials.
The key to good before and after photos is consistency. Make sure you have your setup ready in advance so that you can build a unified portfolio of images that truly showcase your work. Here’s what you will need:
- A high-quality digital camera system that you and your staff have learned how to use with a standard focal length
- A tripod to maintain the camera in a consistent position
- A plain backdrop
- Excellent lighting sources (natural light and varied artificial light will make your photos appear inconsistent and less professional)
- Modesty garments for patients to wear when relevant
- Appropriate consent forms for patients to sign before photos are taken
With cosmetic procedures of the face, in particular, good before and after images require nuance and views from various angles. You will need to decide on a regular set of poses for each procedure, as well as establish and mark the distance patients will stand or sit from the camera—consistency in these areas is critical to creating a highly professional portfolio of images.
If space is tight, you may be unable to set up a dedicated “studio” space. You may place tape on the floor in a consultation or treatment room in front of a plain wall to demarcate the location of the camera and the patient to maintain consistency. Finally, test your setup with staff so that you can seamlessly integrate before and after photos into your pre-operative and follow-up patient appointments.
6. Retrain or hire staff to be sure your team is ready to serve cosmetic patients
Staffing needs at a cosmetic practice are somewhat different. Most cosmetic surgeons employ a knowledgeable, caring patient care coordinator to usher patients through their journey and answer questions that do not require a licensed medical professional. Your nursing and operating room staff must also be trained and prepared to handle cosmetic cases.
Be sure not to overlook the importance of training your front desk staff in serving aesthetic patients; they will be the first voices that patients hear when considering you for their cosmetic procedure. An experienced cosmetic practice consultant can offer detailed advice on handling patient inquiries and receiving patients in the office; applying these principles can notably increase consultation to surgery conversion rates.
Be sure not to overlook the importance of training your front desk staff in serving aesthetic patients.
7. Make sure your office space appeals to aesthetic patients
A key difference between aesthetic patients and those you will see for functional procedures is that they have a choice in who performs their surgery. Entering a comfortable, appealing, and professional-looking space helps patients feel valuable and cared for, and can help them trust that you will listen to their needs and achieve ideal results for them.
8. Retool your marketing to be geared towards cosmetic procedures
Be sure your marketing gives patients an accurate representation of the procedures you offer. As most patients are in search of a specialist, you will only attract new cosmetic patients if it is clear that your focus is on cosmetic medicine and are highly capable of delivering attractive results. Outdated or low-quality websites, Google listings, poor quality patient photos, or association with past practice names may cast doubt in a patient’s mind about your level of dedication to facial cosmetic surgery.
Learn more about specializing in facial cosmetic surgery
If you are an oral and maxillofacial surgeon with ample evidence of facial cosmetic surgery experience, you may qualify to petition the American Board of Facial Cosmetic Surgery (ABFCS) for board certification through the experience route.
Types Of Sinus Surgery
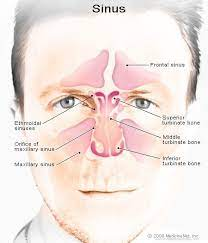
Chronic sinus issues can disrupt quality of life. Swollen sinuses can reduce the airflow, cause snoring, or sleep apnea. The first line of treatment from an ENT specialist is treating your allergies or prescribing antibiotics. Severe cases that don’t respond to this line of therapy aren’t at a lost cause sinus surgery allows doctors to operate on the nose and sinus cavities to improve performance and realign the structure. We identify why and what types of surgeries are available to patients.
What is Sinus Surgery?
Sinus surgery is a group of procedures available to ENTs to help patients find relief from recurrent sinus infection or symptoms. Sometimes patients with abnormal growths or structures don’t respond well to allergy treatments or antibiotics. Both methods are the first call to action to help patients find relief. In the event that non-surgical treatments don’t relieve the problems, sinus surgery allows the doctor to open pathways and improve airflow.
Why Would I Get Sinus Surgery?
Several conditions would require the use of sinus surgery to help alleviate symptoms. The most common would include sinusitis. Sinusitis is the swelling of the passages and sinuses that result in a stuffy nose, pressure in the nose, eyes, and forehead, coughing, nasal drainage and more.
Another common reason for surgery is a nasal polyp. Enlarged polyps or clusters of polyps are swelling of the nasal lining inside the nose. If they expand a person can experience a reduced sense of taste and nasal blockages that could infect the sinuses.
Deviated septums block one side of the nose causing a reduction in air flow. Treatments exist to reduce the swelling of the nasal tissue that could contribute to the deviation, but in some instances when the patient doesn’t respond, surgery helps restore balance to airflow.
Types of Sinus Surgery
SEPTOPLASTY
Septoplasty is an outpatient procedure aimed at correcting issues related to the midline of the nose. The process restructures the partition that divides the nostrils called the septum. The septum is made from both bone and cartilage. Its purpose is to aid in moving the air we breathe into the lungs. Without it, the air could remain in the nose. Either from a congenital disability (the nostril pressing against the birthing cavity at birth) or possibly an injury (a broken nose for example), the septum can obstruct the airflow and significantly disrupt the amount of air inhaled through the nose.
Anyone who suffers from chronic sinusitis has the compounding issue of congestion and a deviated septum. Septoplasty attempts to redirect the alignment and open the air passages back up by restructuring the bone and cartilage.
TURBINATE REDUCTION
The turbinates inside the nose can become swollen and inflamed from infection, irritation, or allergies. Any of these symptoms could cause nasal obstruction and lead to excess production of mucus. Too much mucus and you have congestion. Three turbinates exist inside the nasal passage: the upper, middle, and lower. Their purpose is to humidify, warm, and filter the air we breathe. They are composed of a bony structure surrounded by tissue and a mucus membrane.
Turbinate reduction aims to reduce the size and swelling making it easier to breathe. The procedure often requires the use of radiofrequency. It involves the insertion of a needle-like instrument into the turbinate. The radio frequency is transmitted into the tissue causing “controlled damage.” As the nose starts to heal, the turbinate begins to reduce in size. Undergoing turbinate reduction surgery does not affect the size or shape of the nose, and patients shouldn’t experience any long-term side-effects.
FUNCTIONAL RHINOPLASTY
Two kinds of rhinoplasty exist: cosmetic and functional. Rhinoplasty at its core is a procedure that restructures the bones and cartilage that make up the nose. Functional rhinoplasty is performed by ENT surgeons with the expressed interest of helping the patient remove abnormalities that cause issues with breathing. Everything from the shape of the nostrils to the angle of the nose participates in airflow being directed into the lungs. Obstructions that are treatable with antibiotics, allergy treatments, or other less invasive methods respond well to functional rhinoplasty. During the procedure, the doctor will resculpt bone and cartilage that sometimes result in a change in nose shape. Doctors can operate by working from inside the nose making a small incision or the outside of the nose.
BALLOON SINUPLASTY
Balloon sinuplasty is a less invasive procedure designed to help patients find relief from chronic sinusitis symptoms. The method is a straightforward application wherein the doctor inserts a flexible balloon catheter into the sinus passage. The process is aided by a tiny wire with a flashlight on the end to help navigation. Once the balloon is appropriately positioned, it’s slowly inflated to open up the sinus cavity. The doctor uses a saline solution to help flush out the mucus and pus. Many patients feel an instant relief in pressure once the fluid starts to drain. The gentle pressure of the balloon against the sinus cavity helps to restructure the bones and cartilage. After its removal, the sinuses should feel clearer.
FUNCTIONAL ENDOSCOPIC SINUS SURGERY (FESS)
Maybe one of today’s most common sinus surgery options, FESS is a procedure that utilizes a magnifying endoscope to both view the sinuses and remove any affected tissue or bone. It’s reconstructive to open the connection between the sinuses and nose. The result should produce better drainage, reduce blockages and flush out infected material while maintaining healthy tissue for the nose to operate normally. As the name suggests, the procedure is endoscopic. Your ENT surgeon makes small incisions inside the nose to allow for a small tube with a camera and light at the end (endoscope) to survey the inside of the nasal cavity. FESS is often performed in conjunction with other sinus surgery options like septoplasty.
Middle Tennessee Sinus Surgery Options
Each procedure for sinus surgery comes with minimal risk factors or long-term side-effects. But, surgery is still surgery, and you want to be in the best hands. Working with Board Certified ENT specialists like OAT is one of the most effective ways of ensuring your procedure goes smoothly and achieves the best results. If you suspect issues with your sinuses, contact OAT today to schedule an appointment.
Before and after sinus surgery
Chronic sinusitis is an illness characterized by prolonged infection and inflammation of the lining of the nose and the sinuses. Patients with chronic sinusitis experience a variety of symptoms, including facial pressure, nasal congestion, discolored nasal discharge, and “post-nasal drip.” A diagnosis of sinusitis should be made only after careful evaluation by your doctor. For the majority of patients with sinusitis, infections can be successfully treated with medications. For a small percentage of patients, however, infections recur or persist even after long courses of medication. Such patients often benefit from surgery. After reviewing your medical history and x-ray studies, your ear, nose, and throat specialist can determine if you are a surgical candidate.
What is Endoscopic Sinus Surgery?
Endoscopic sinus surgery is a procedure designed to open the natural drainage pathways of the sinuses to restore their function and health. In chronic sinusitis, the sinuses are unable to drain adequately due to inflammation of the narrow drainage pathways. As a result, nasal secretions can become trapped in the sinuses and become chronically infected.
The goal of surgery is to carefully remove the thin, delicate bone and mucous membranes that block the drainage pathways of the sinuses. The term “endoscopic” refers to the use of small fiberoptic telescopes that allow all of the surgery to be performed through the nostrils, without the need for any skin incisions. Endoscopic sinus surgery is generally performed on an outpatient basis.
What to expect before, during, and after surgery?
Before Surgery: In preparation for your surgery, your physician may prescribe preoperative medications to optimize the condition of your sinuses for surgery. The medications may include antibiotics and/or oral steroids. Please be sure to start any preoperative medications on the appropriate day and adhere closely to the prescription. In addition, you should avoid taking the following medications for at least fourteen days prior to surgery: aspirin, ibuprofen (Motrin/Advil), naproxen (Aleve), other non-steroidal anti-inflammatories (NSAIDS), vitamin E (multivitamin is OK), gingko biloba, garlic (tablets), and ginseng. These medications can thin the blood and create excessive bleeding. Tylenol is safe and may be taken anytime up to the day of surgery. St. John’s wort should also be avoided for 2 weeks prior to surgery because of possible interactions with anesthesia medications. If you take the blood thinner Coumadin, please discuss discontinuation of this medication with your surgeon.
If you smoke, it is critical that you stop smoking for at least three weeks prior to surgery, and at least four weeks after surgery. Smoking can contribute to scarring, poor healing, and failure of the operation. Your primary care physician can direct you to resources for smoking cessation. Finally, it is important to inform your primary care physician that you are planning to have sinus surgery. Your primary care physician can help to clear you medically for surgery. Most of the necessary pre-operative testing will be performed at Stanford on the day of your preoperative visit, but occasionally we will request old records from your primary care physician. We will make every effort to keep your primary care physician informed regarding your medical status both before and after your surgery.
During Surgery: In most cases, you will receive general anesthesia for your surgery, which means you will be asleep for the entire procedure. However, if you have a preference for local anesthesia, please let your doctor know as this may also be an option in some cases. After your surgery has been completed, you will spend about one hour in the recovery room, followed by an additional recovery period of 1-2 hours in the second stage recovery unit. Most patients feel well enough to go home the day of surgery. You will most likely go home without nasal packing.
After Surgery: You can expect mild bleeding for 1-2 days after surgery and a general sense of fatigue for 1-2 weeks after surgery. In general, pain can be successfully controlled with narcotic or non-narcotic medications. For more details about postoperative care, please see the separate guide, “Postoperative Care Instructions.” You will have a series of postoperative visits that are critical for a successful outcome. At each visit your doctor will perform a procedure called nasal endoscopy to check how the sinuses are healing. An additional procedure called debridement may be necessary in order to clean blood from the sinuses and prevent early scar tissue formation. (Please note that these procedures are not included in the surgical charge and thus are billed separately.) Your visit schedule will usually consist of 3 visits over the first 6 weeks. Thereafter, your visits will be spaced a few months apart, depending on how well your sinuses are healing.
Risks of Surgery
As with any surgical procedure, endoscopic sinus surgery has associated risks. Although the chance of a complication occurring are very small, it is important that you understand the potential complications and ask your surgeon about any concerns you may have.
- Bleeding: Most sinus surgery involves some degree of blood loss, which is generally well tolerated by the patient. However, on occasion, significant bleeding may require termination of the procedure. Although most patients do not require nasal packing, a few patients will require a small nasal pack or tissue spacer to be removed after one week. Blood transfusion is rarely necessary and is given only in an emergency.
- Recurrence of disease: Although endoscopic sinus surgery provides significant symptomatic benefits for the vast majority of patients, surgery is not a cure for sinusitis. Therefore, you can expect to continue with your sinus medications even after successful sinus surgery, although in general your requirements for such medications should be lessened. In some instances, additional “touch-up” or revision surgery may be necessary to optimize your surgical outcome.
- Spinal fluid leak: Because the sinuses are located near the brain, there is a rare chance of creating a leak of spinal fluid (the fluid lining the brain) or injuring the brain. Should the rare complication of a spinal fluid leak occur, it may create a potential pathway for infection, which could result in meningitis. If a spinal fluid leak were to occur, it would require surgical closure and hospitalization.
- Visual problems: Visual loss has been reported after sinus surgery due to injury to the eye or optic nerve. The potential for recovery in such cases is not good. Fortunately, such a complication is extremely rare. Injury to the eye muscles may result in double vision. Persistent tearing of the eye is another possible complication. Tearing problems usually resolve on their own but occasionally require additional surgery.
- Other risks: Other uncommon risks of surgery include alteration of sense of smell or taste; persistence and/or worsening of sinus symptoms and facial pain; change in the resonance or quality of the voice; and swelling or bruising of the area around the eye.
Some patients have a crooked nasal septum (“deviated septum”) that needs to be corrected at the time of surgery through a short procedure called septoplasty. This procedure is performed through a small hidden incision and involves dissolvable stitches that are hidden in the nostril area. If you require septoplasty, there are additional risks associated with this procedure. The primary risks are bleeding or infection in the area of the septum; numbness of the front teeth; the development of a hole through the septum (septal perforation); brain fluid leak; or recurrence of septal deviation. There is a very small risk that such occurrences could alter the external appearance of the nose.
Restrictions during postoperative recovery period
For the first week following surgery you should not blow your nose. In addition, you should not bend, strain, or lift more than 20 lbs. during the first week. Light walking and regular household activities are acceptable anytime after surgery. You may resume exercise at 50% intensity after one week and at full intensity after two weeks. You should plan on taking one week off from work and ideally have a half-day planned for your first day back.
Conclusion
We at the Stanford Sinus Center are committed to providing you with the highest level of care in a comfortable and caring environment. We want you to have as complete an understanding as possible about your sinus condition and about our recommendations for treatment. Please feel free to ask questions about