How Will Insurance Cover Breast Reduction
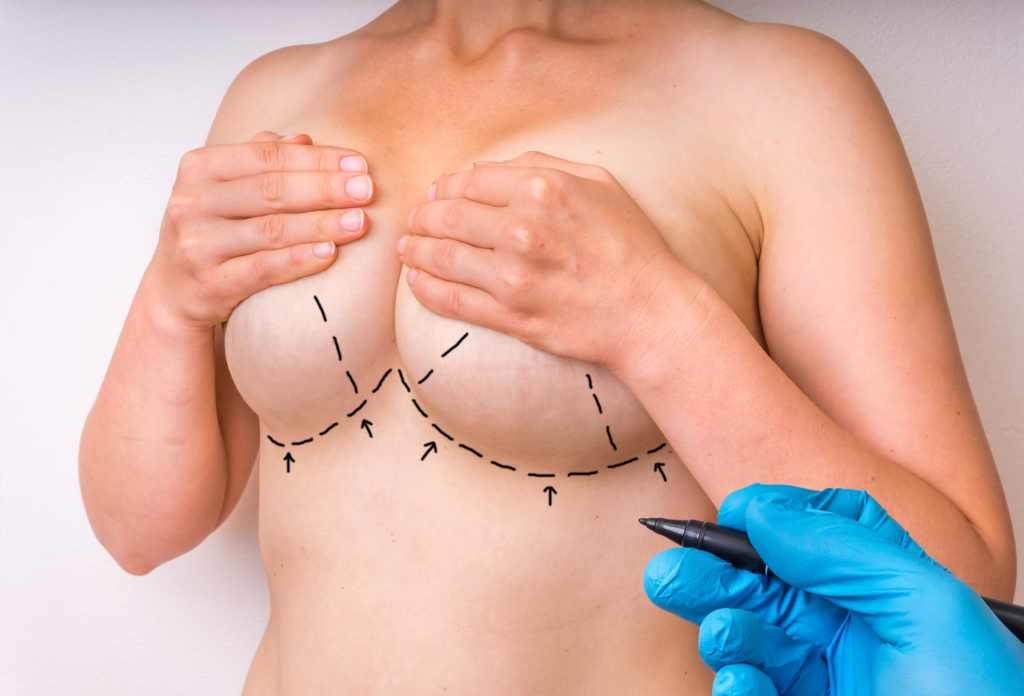
Even though it’s one of the most often performed cosmetic procedures in the US, breast reduction surgery is still widely misunderstood. Reducing the size of one’s breasts through surgery might make them more proportionate. Women with painfully big breasts are the most common candidates for this procedure. Nonetheless, many women who are otherwise happy with their breasts are considering surgery to make them smaller and more symmetrical.
Surgical removal of fat and tissue from your breasts (glandular excision) is still regarded the “gold standard” for breast reduction surgery, despite the fact that there are various other types of breast reduction techniques available today. Around 70% of breast tissue is removed during the treatment, leaving only the skin, blood arteries, and muscles that support the breasts. If your surgeon notices that you have extra fat deposits in the chest or back, he or she may suggest liposuction as a subsequent procedure.
Breast reduction is a surgical procedure that is intended to reduce the size of the breasts of an individual. It may also be referred to as a mastopexy, or surgical breast reduction. In this procedure, excess skin and fat are removed from the breasts to give them a flatter appearance. Read on to learn more on Does Medicare Cover Breast Reduction and breast reduction requirements weight.

How Will Insurance Cover Breast Reduction
Very large breasts — sometimes called macromastia — can cause health problems. The weight of the breasts may lead to pain in the back, shoulder, and neck. Some women have permanent shoulder grooves caused by bra straps or recurrent rashes under the breasts.
Breast reduction surgery — also called reduction mammoplasty — can not only remedy physical symptoms like these but also have psychological benefits. It can improve people’s quality of life, self-esteem, and body image.
If you’re considering a breast reduction, you’re probably wondering how much it costs and whether health insurance covers it. Breast reduction surgery for cosmetic reasons doesn’t qualify for coverage. But if you’re getting the surgery for medical reasons, your health insurance may well cover it. Your insurer has specific rules for how you can get coverage for a breast reduction.
Read on for more details about the cost of breast reduction surgery and when insurance will pay for it.
Is breast reduction covered by health insurance?
It depends. Health insurance only covers breast reduction if it’s considered medically necessary to treat chronic health symptoms.
This means that before you can schedule the breast reduction surgery, you’ll probably have to get insurance authorization. The insurance company will require your surgeon to submit certain health records on your behalf; it will then assess your medical need for the surgery. (Even if your insurance does cover the surgery, you’ll still have to pay copays or deductibles.)
If your breast reduction surgery doesn’t meet your health plan’s medical necessity criteria, it will be considered cosmetic, meaning the insurance company won’t cover it.
How to get a breast reduction covered by insurance
Getting approval for breast reduction surgery can be a long, complicated process. Insurers have different criteria for judging the surgery as medically necessary.
Your health insurance plan may require:
- A physician’s letter detailing your health symptoms and how long you’ve had them
- Medical records of previous treatments you’ve tried
- Your height and weight
- Photos of your breasts
You’ll generally have to provide records showing that:
- You have chronic health symptoms caused by having large breasts
- You have tried other, nonsurgical treatments
- The nonsurgical treatments have not helped
Some insurers have required a person to be within 20% of their ideal body weight before approving coverage, as weight loss alone can cause the breasts to become smaller. However, this requirement has been questioned by some surgeons and academics, given that lasting weight loss is difficult and sometimes unrealistic.
Your best bet is to contact your insurer as early as possible, and ask them to list and explain all the requirements and what forms of proof they will accept. That way, you’ll know exactly what documentation to gather and submit.
What makes a breast reduction medically necessary?
A doctor must determine that the surgery is medically necessary. You may need to provide evidence to the doctor and insurer that you’ve already tried nonsurgical treatments — such as physical therapy, weight loss, or musculoskeletal treatments — without success. The insurance company may want proof that you’ve had symptoms for at least 6 months.
Insurance companies may approve breast reduction surgery as medically necessary if:
- You have severe rashes or skin infections that are hard to treat.
- Your physical activities are restricted.
- You have nerve compression due to the weight of the breasts.
- The weight of your breasts is significantly affecting your posture and spine alignment.
- Your breasts are painful.
- You have upper-back, neck, or shoulder pain.
- You have shoulder grooves from bra straps.
Do breasts have to be a certain size in order for you to be a candidate for reduction?
When it comes to reduction surgery, it’s not exactly a matter of how large your breasts are. The main measure is the amount of tissue to be removed. Your insurance company’s “medically necessary” criteria may require that the procedure remove a certain minimum amount of tissue.
Some insurers use the Schnur Sliding Scale as a reference. This is a ratio that compares the weight of the removed breast tissue with your total body surface area. Although this calculation is a common guideline, it’s not always an absolute rule.
Typically, if your Schnur ratio is above the 22nd percentile, your surgery is considered medically necessary. If it’s below the 5th percentile, it’s considered cosmetic. If your ratio is in between, it may be considered either medical or cosmetic, or a mix of both, and may or may not be approved by insurers.
How much weight is removed in breast reduction?
The minimum amount varies according to your insurance carrier’s definition. For some, if the amount of breast tissue removed is less than 200 to 350 grams (7 to 12 ounces), the procedure may be considered a breast lift rather than a breast reduction. A breast lift is typically considered cosmetic surgery, and so it is not covered by insurance.
Does Medicare pay for breast reduction?
Not always. Like private insurers, Medicare doesn’t cover cosmetic breast reduction surgery. Both original Medicare and Medicare Advantage will cover the procedure when it is determined to be medically necessary. However, you will probably have to pay for a deductible, copay, or coinsurance.
How much does a breast reduction cost with insurance?
The total cost of breast reduction surgery has several components, including:
- Surgeon’s fee
- Anesthesia fees
- Hospital costs
- Medical tests
- Post-surgery garments
- Prescription medications
The average plastic surgeon’s fee for breast reduction was $5,717 as of 2020, according to the Aesthetic Plastic Surgery National Databank. But fees vary significantly depending on factors like:
- The surgeon’s level of experience
- What breast reduction technique the surgeon uses
- Whether you have the surgery on one or both breasts
- Market pricing in your geographic location
For example, according to estimates from FAIR Health, here’s a cost breakdown for a patient in Columbus, Ohio, with commercial insurance.
| Item | Price |
|---|---|
| Surgeon’s fee | $4,782 ($2,391 per breast) |
| Anesthesia fee | $997 |
| Facility cost for ambulatory surgical center | $6,548 |
| Facility cost for hospital outpatient | $10,257 |
| Total | $12,327 at an ambulatory surgical center or $16,036 at a hospital as an outpatient |
How much does breast reduction surgery cost for the uninsured?
Without insurance, that patient in Columbus, Ohio, would face costs like this, according to FAIR Health:
| Item | Price |
|---|---|
| Surgeon’s fee | $15,870 ($7,935 per breast) |
| Anesthesia fee | $2,151 |
| Facility cost for ambulatory surgical center | $16,582 |
| Facility cost for hospital outpatient | $20,179 |
| Total | $34,603 at an ambulatory surgical center or $38,200 at a hospital as an outpatient |
How can I finance a breast reduction?
Numerous plastic surgery providers offer medical financing options, including payment plans. Many accept CareCredit, a healthcare credit card. CareCredit has promotional plans that feature no-interest financing if you pay in full within a given period (6 to 24 months). If you don’t, however, interest charges kick in — potentially at the high annual percentage rate (APR) of 26.99%.
Some online lenders offer loans that can be used to pay for plastic surgery. For example, Prosper Healthcare Lending loans have interest rates ranging from 7.95% to 36.00% APR for up to 60 months.
Of course, you don’t have to use a loan or credit card marketed specifically for healthcare to finance a breast reduction. You can use savings, or shop around to get the lowest-rate loan or credit card available to you. The national average APR on credit cards is less than 15%.
What to expect after breast reduction surgery
After breast reduction surgery, you may need to take a week or two at home to rest and recover. You’ll have some appointments with your plastic surgeon to remove your sutures and get follow-up care. It may be a month or more before you can exercise or do any strenuous activity.
What are the potential complications of breast reduction surgery?
Like any other major surgery, breast reduction surgery has risks. These can include:
- Bleeding
- Infection
- Adverse reaction to anesthesia
- Bruising
- Scarring
- Loss of sensation in the breasts or nipples
- Difficulty or inability to breastfeed
- Asymmetric breasts, potentially requiring additional surgery
Even if your incisions heal without mishap, the results might not turn out looking exactly as you envisioned or as your surgeon planned. This is a risk with any type of plastic surgery.
Breast reduction surgery is covered by health insurance when it’s medically necessary. Proving the medical necessity to your insurer can be complicated and may require a lot of documentation from your healthcare provider. Uninsured people, or those who want the reduction for aesthetic reasons, will have to pay for it entirely out of pocket.
Does Medicare Cover Breast Reduction
Medicare only covers breast reduction surgery if it is medically necessary. Medicare does not cover elective cosmetic breast reduction. Patients can get coverage under Medicare plan if it is deemed as a medical necessity, you have a valid referral and meet strict criteria.
There are several health concerns that can help qualify you for Breast Reduction Surgery and make it medically necessary including:
- Chronic skin infections due to larger breasts. The common one is intertrigo.
- Relief from body pain; back pain, neck pain or shoulder pain
- To remedy other health conditions that affect your quality of life
Quick Facts about Medicare Cover for Breast Reduction
- Medicare only covers breast reduction surgery if it is medically necessary.
- Medicare does not cover elective cosmetic breast reduction.
- Patients can get coverage under Medicare plan if it is deemed as a medical necessity, you have a valid referral and meet strict criteria.
What is Breast Reduction Surgery?
Breast reduction is a surgical procedure that reduces the size of your breasts by removing excess fat, tissue, and skin. It is an ideal procedure for anyone who has large breasts that look out of proportion to the rest of their body. Heavy breasts can lead to skin infections, neck, back and shoulder pain.
Why Should I Consider A Breast Reduction?
Breast reduction is truly a life-altering procedure. The surgery can prevent and treat plenty of recurring problems that come as a side effect to having larger breasts and give you a better quality of life.
Most of the patients feel extremely confident and happy post the surgery. It is almost like they have a new outlook on life and are able to dive into a wide range of physical activities. Moreover, the surgery also improves self-confidence and body image.
With the new confidence and body, you will be able to rock all those clothing options that you previously didn’t. Trust me, it is one of the most fun advantages of getting the surgery.
Research shows that woman’s health improves significantly post-reduction mammoplasty. Neck pain, back pain, shoulder pain, infections and rashes will be completely gone after getting the procedure done.
You’ll need a Medical Referral with Documented concerns
In order to claim your surgery on Medicare, you will need a Medical Referral from your General Practitioner. You can get it prior to booking an initial consultation with a cosmetic surgeon or after the first appointment.
It is important to demonstrate medical necessity, including pain in the neck and/or shoulder region. While consulting with your GP, it is worth discussing your symptoms to ensure the clinical need is documented in your referral.
So will my Breast Reduction be covered by Medicare?
The answer to this is ‘MAYBE’ – Medicare offers rebates on breast reduction procedures if you meet the special criteria and conditions as listed below.
How Do You Qualify for Medicare Rebate for Breast Reduction Surgery? – MBS Codes
These MBS Codes may be applicable for Breast Reduction Surgery:
45523 Reduction mammaplasty (bilateral) with surgical repositioning of the nipple:
(a) for patients with macromastia and experiencing pain in the neck or shoulder region; and
(b) not with insertion of any prosthesis
45520 Reduction mammaplasty (unilateral) with surgical repositioning of the nipple, in the context of breast cancer or developmental abnormality of the breast
45522 Reduction mammaplasty (unilateral) without surgical repositioning of the nipple:
(a) excluding the treatment of gynecomastia; and
(b) not with insertion of any prosthesis
What these terms mean:
- Macromastia – the condition of having abnormally large breasts. (Breast Hypertrophy)
- Prosthesis – an artificial body part e.g. a breast implant
- Bilateral – both sides / both breasts
- Unilateral – one side / one breast
- Gynecomastia – Excess Male Breast Tissue
Will Medicare Cover Breast Reduction Surgery for medical reasons? – MBS Criteria
If you have required documentation for breast reduction surgery and you meet the Medicare criteria, you can qualify for a rebate. It is important to note that the recent MBS changes included additional photographic proof, examination evidence, reporting documentation, and stricter patient criteria for Medicare rebates.
Your eligibility will essentially be based on the following Medicare criteria;
(a) for patients with macromastia (large breasts) and experiencing pain in the neck or shoulder region; and
(b) not with insertion of any prosthesis – this means you cannot have an implant put in when having the reduction to be able to claim the rebate
What are the Medicare breast reduction criteria in Australia?
How do I qualify for the coverage of Medicare Breast Reduction?
You can qualify for breast reduction coverage if you meet Medicare’s criteria.
If you’re having breast reduction due to excessive pain, you’ll be required to meet multiple conditions. In this case, your doctor needs to verify that:
- Surgery is essential to treat the pain
- Other non-surgical treatments haven’t worked for you in the past
- You are having persistent pain for a minimum of six months
There are certain cases when the pain is caused by a specific breast condition such as breast hypertrophy. Hypertrophy causes your breasts to increase in size which causes pain and a variety of other problems. Medicare will cover the cost of breast reduction if your doctor indicates that pain is caused by hypertrophy.
MBS Item Number 45523
- Reduction mammaplasty (bilateral) with surgical repositioning of the nipple:
- (a) for patients with macromastia and experiencing pain in the neck or shoulder region; and
- (b) not with insertion of any prosthesis
MBS Item Number 45520
- Reduction mammaplasty (unilateral) with surgical repositioning of the nipple, in the context of breast cancer or developmental abnormality of the breast
MBS Item Number 45522
- Reduction mammaplasty (unilateral) without surgical repositioning of the nipple:
- (a) excluding the treatment of gynecomastia; and
- (b) not with insertion of any prosthesis
Will health insurance help cover the cost of the Breast Reduction surgery?
You need to meet strict criteria for your insurance or Medicare to pay for the surgery. It is important to be fully aware of Medicare codes and rebate eligibility criteria as these two factors will change/affect your claim.
If you qualify for Medicare you may also be eligible for rebates on the Reduction surgery from your Private Health Insurance Provider. This only applies if your condition meets the criteria for Medicare Item Number.
For most breast reduction surgeries, Bronze Hospital cover is enough. In some cases, Silver Hospital cover might be required as well. It is important to check directly with your own Private Health Fund, regarding your policy as they can differ.
Why is the Medicare Rebate for Breast Reduction Confusing?
This is due to the variables of the situation. Each patient is different and has different reasons for getting the surgery done.
In some cases, Medicare offers a minor rebate on certain procedures. It is important to note that rebates are generally available for reconstructive plastic surgery only if the surgery is deemed ‘essential’. For a lot of patients, breast reduction will be under this category.
When it comes to Plastic & Cosmetic Surgery, the Medicare REBATE guidelines are quite clear. Medicare does not cover ‘non-therapeutic cosmetic surgery’ NOR ‘non-therapeutic plastic surgery’ procedures. Significant Breast Ptosis after pregnancy, Chronic Back Pain, and skin infections related to large breasts are chronic medical conditions.
NOTE – Medicare Rebates are subject to change and review
Please note that MBS Item codes are reviewed regularly and can be changed/eliminated from the Medicare rebate schedule at any time. If you are currently eligible for a Medicare rebate for breast reduction surgery, it is best to get the procedure sooner rather than later.
Will my private health fund cover my breast procedure?
Private Health Funds only cover a procedure if;
- The patient meets current Medicare eligibility criteria and has an MBS item number.
- You need to meet the strict criteria for Medicare rebate to quality for health fund cover and provide proof.
- Extensive documentation, examinations, imaging or volumetric testing, and photographs are required to substantiate a claim.
How much will my Breast Reduction cost if self-funded?
The cost of having a Breast Reduction performed by a Specialist Plastic Surgeon in Australia varies depending on the area, experience and expertise of the surgeon, and your unique needs.
It is primarily because the breast reduction procedure is customized to suit the needs of an individual and the desired outcome.
You can contact Dr Turner’s team for an estimate or come for a consultation to get a quote. We will also help you understand the costs and risks associated with the surgery. Our team can also help you access your eligibility for coverage by MBS or your health fund.
In order to access your eligibility to claim a Medicare rebate for your Breast Reduction Surgery, visit your GP or other specialist and ask for a referral to Dr Turner. You will need a valid referral at the time of surgery. A GP referral lasts for 12 months.
You can also speak to our knowledgeable Patient Care Team, who are available to answer your questions.
Can I Use My Super Fund to pay for Breast Reduction Surgery?
Some patients use their own super fund to pay for their breast reduction surgery. Before requesting the early release of funds, it is very important to note that:
- Each application for early Super release is assessed on an individual basis and financially assessed.
- Superfund withdrawal applications can be made through your MYGOV account via the ATO.
- Tax implications apply. The withdrawal may be taxable. Hence, it is important to seek professional financial advice.
Breast Reduction Medicare FAQs

How can I get a breast reduction with Medicare?
It is possible if your breast reduction surgery is a medical necessity and you meet the strict criteria that Medicare will pay for the procedure. The first step is to visit your GP and get the documentation that supports the ‘necessity’ element of the medicare surgery. Then call Dr Turner.
What qualifies a woman for breast reduction?
You are most likely an ideal candidate for breast reduction if:
- You are physically healthy with no chronic illnesses
- You have realistic expectations from the treatment
- You don’t smoke or can quit it for the specified interval
- You are bothered by feeling that your breasts are too large in comparison with the rest of your body
- You have limited physical activity due to large breasts
- You experience back, neck and shoulder pain that is caused by the excessive weight of your breasts
- You get shoulder indentations from wearing a bra
- You experience skin irritation beneath the breast crease due to rubbing of the skin
- Your large breasts are impacting your day to day life.
This article focuses solely on how to put contact lenses in small eyes. There are a few suggestions you should consider every time you try to put the lenses on. First of all, wash your hands before we continue and dry them. Now we can start.
The first part of this article focuses on soft contact lenses and the different techniques you should consider. In the second part, I will give you my tips for rigid contacts.
Before you begin with the lens right away I advise you to first place your fingers without the lens. I assume you are right-handed. If you are left-handed you can just inverse my recommendations. Prepare a towel and a mirror before you begin. A white towel comes in handy to locate the lens faster when you drop it. In addition to that, a lot of my clients find it easier to try the contacts in front of a mirror.
Place Your Fingertips Correctly
This part is critical! Make sure to place your fingertip right on the spot where your eyelashes sit. First, do this with your lower lid with the middle finger of your right hand. Then take the left hand and place the middle finger of your left hand right where the lashes are on the upper lid. Just watch the pictures below.
This will clear things up for you. When you grab your upper eyelid make sure to not go come from the side with your hand as this approach will give you less space to handle the contact lens in front of your eye. grab your upper lid and place your left hand in front of your forehead.
Ok perfect now you know the perfect spot where you should place your fingers. with this placement of your fingers, you will not be able to blink anymore. If you place your fingers a little above and below your eyelashes you will be still able to blink which makes it a lot harder to put the contacts on your eyes.
Just for practicing purposes pull on your lids so you can see the white parts of your eyeball above and below the iris. This pulling force needs to be kept up during the whole setup until the lenses sit on your eyes. So constantly remind yourself “Pull the lids out of the way, pull…pull and again pull”. This is also what I say to my clients constantly when they are in my shop and get the contact lenses fitted for the first time.
Breast Reduction Requirements Weight
Some insurance companies will deny breast reduction surgery unless the BMI is <30, others <35, while others need to see documentation that the patient has attempted to lose weight in the past through diet, exercise or weight loss surgery. This is because breast size may decrease with weight loss.
Insurance companies have a variety of criteria that they use to determine if a breast reduction will be covered by your plan. It is also important to remember that these criteria may change from year to year. Although an insurance company may be known to cover a certain procedure, they may have negotiated specific contracts with specific exemptions with your employer that could have excluded a breast reduction.
Your insurance company may wish to learn about some or all of the following criteria to determine if your procedure will be covered:
1. Signs and symptoms for which a breast reduction may be medically indicated. Insurance companies assign specific numeric codes to medical problems or symptoms called ICD-9 (International Classification of Diseases) codes. Large breasts (ICD-9: 611.1) can cause postural backaches (ICD-9: 724-5, 781.9), and upper back and neck pain (ICD-9: 724.1, 723.1). Skin irritation referred to as intertrigo (ICD-9: 695.89) as well as pressure leading to ulnar nerve parasthesias or numbness (ICD-9: 782.0) may also be related to excessively large breasts.
2. Body mass index (BMI). This is a number that is used to determine your weight status. It correlates your height and weight and should be used as a general guideline only. See the bottom of this document for information on the BMI and how to calculate it.
Some insurance companies will deny breast reduction surgery unless the BMI is <30, others <35, while others need to see documentation that the patient has attempted to lose weight in the past through diet, exercise or weight loss surgery. This is because breast size may decrease with weight loss.
3. Weight of breast tissue removed. Most insurance companies will want to know the weight of breast tissue the plastic surgeon believes he or she can remove during a breast reduction. This number may be 450 grams, 500 grams or 600 grams. Some companies have a more detailed approach to avoid penalizing patients who are of smaller stature but who have proportionately smaller breasts. These companies will correlate the body surface area (BSA) with the weight of the specimen removed. So, in these cases, for small individuals the amount of volume that needs to be removed for coverage may only be 325 grams, whereas for larger individuals this weight may need to approach 1,000 grams.
4. Breast reduction to match a breast treated for breast cancer. A breast reduction is also covered if it is to balance a healthy but larger breast with the other breast that has been affected by breast cancer and its treatment. This is protected by the Women’s Health and Cancer Rights Act of 1998. This ensures reconstructive treatment of the affected breast as well as balancing procedures to match the healthy breast to the reconstructed breast. This may include a breast reduction of any size.
5. Supportive letter from another physician or health care provider. Although a plastic surgeon should perform your breast reduction, he or she is likely to have just met you for the first time during consultation. Your insurance company may request supportive letters from other health care providers to support the request that a breast reduction will treat your medical symptoms. This supportive letter may also serve to document that attempts at weight loss, exercise and physical therapy have already been made to treat the symptoms of excessively large breasts. It may also be necessary to document cases of rashes or intertrigo
Now pull on your lids and try to place the contact lens right on your cornea. You can even place the lens on the white of your eyeball and it will automatically make its way in the middle of your eyes after you blinked a few times. This sounded easy but in reality, you will experience this:
- The contact lens falls down
- The contact lens does not snuggle on your eye but rather sticks to your finger
- The contact lens sits upended on your eye because your lids pushed it this way
- The contact lens sits on your eyelashes
So in reality you will oftentimes need up to an hour before the contact lens sits on your eye. Especially when you have small eyes the process is a little harder and will take more time. Make sure to get your eyes a little rest after you tried it a few times.
The mentioned bullet points are usually caused because your eyelashes hindered you to place the contact lens on your eyes correctly and they had a few seconds to snuggle on your eye. Make sure you pull on the lids permanently when trying to place the contacts on your eye. This is key. Pull, pull and pull and give the lens at least three seconds when you feel the lens on your eyeball.
This process should be repeated until the lenses sit on your eye. There are also a few ninja optician tips you can try for extra small eyes I will mention below but first, the already mentioned basics need to be set before you try my ninja optician tips below.
If you place your fingers in the positions mentioned before and you still can’t open your eyes wide enough for a contact lens it is time to sneak the contact lens under your lids. You normally place the contact lens on the fingertip and the soft contact lens has a diameter of approximately 0,55/inches 14mm when it is unfolded on your eye. But when you push the contact lens a little with your thumb you can reduce the size a little so you can slide the lens under your lid.
Ninja Optician Tipps for Extra Small Eyes
One word of caution though. Try not to force the contact lens in your eyes. When I say slide them under your lid I really mean do it in a gentle way and give the contact lens enough time to snuggle on your eye. When you push the lens a little to make the vertical diameter smaller the probability is a little higher for the contact lens to not unfold on your eye.
When this happens you will experience discomfort and need to pull the lens out.
When problems with contact lenses and extra small eyes come up it also helps to record yourself from the side with your smartphone. This way you can see where you are looking when trying to get the contact lens on your eye. This is important because when move your eyeballs constantly before the contact lens has enough contact with its surface the lens can not settle correctly.
The Diameter of the Contact Lens
Above I mentioned the average diameter of a soft contact lens. However, if you can not put the contact lens on your eyes even after a few sessions I would recommend smaller contact lenses. In some cases, individual soft contacts can work but in most cases, rigid gas permeable contact lenses will be even smaller as those usually only cover a part of your cornea.
So with a smaller lens, you should have an easier time putting the lens on even with smaller eyes. The placement of rigid contact lenses is even more important in the first place because they need to be placed right on your cornea when you put them in. In some cases, it is easier to look a little up or down so your lids are as far away as possible from the lens so you can place them as easily as possible on your eyes. Just look at the pictures below and things will get a lot clearer for you.

I hope the instructions here led to success the next thing will be to put them out. Especially with smaller eyes, this can be an issue too. So if you are struggling to remove the contact lenses I have the next article ready for you here.
I wish you a great day.
Tricks to putting in contacts
Wearing contacts gives you great freedom over glasses, but for many, the struggle and frustration of learning how to insert and remove contact lenses is too much. Here’s your expert guide to worry-free contact wear, complete with troubleshooting for common contact-wearing problems.
1. How to remove a contact lens that “disappeared”
If a contact disappears, it may have fallen onto the floor to be lost forever, but, in some cases, it could still be stuck under your eye. You may feel a prick under your eyelid after a contact has disappeared because the contact has likely folded or otherwise moved out of place on the eyeball.
If you can’t see it, don’t try to lift your lid up enough to grab it because you’ll hurt yourself. Instead, close your eye and look down as far as you can, and then, while still looking down, gently pull the lid up slowly. This dislodges the lens so that you can easily remove it. If this doesn’t work, please contact Dr. Stein for an appointment and he will assist you.
2. How to remove a contact lens first thing in the morning
It’s not advisable to sleep in your contacts, but some contacts are designed for 24-hour wear, making sleeping in them less risky. When you first wake up, your eye may be dry, and the contact may have temporarily adhered to the cornea. Trying to remove it in this state may damage your cornea, so make sure your eye is sufficiently lubricated with eyedrops before removing the contact.
3. What to do if the contact keeps falling out during insertion
The trick is to gently hold the contact on the eye for about 1 second and then very slowly move the eyeball back and forth slightly. This helps the fluids on your cornea pick up the contact from your finger.
Without blinking, move the eyeball slowly down and then around to secure the lens in the eye. Now you can blink, and the lens should stay in place. With practice, this takes fewer than 2 seconds to do.
4. What to do if your contact falls out at an inconvenient time
As a contact wearer, you should always be prepared. Carry a travel-size bottle of saline in your backpack, satchel or purse. Keep a contact case with you at all times. If the contact falls out, don’t attempt to re-insert it immediately. Instead, put some fresh saline into your case, place the contact in there, and then get to the nearest restroom to thoroughly wash your hands and the contact before reinserting.
Never rinse contacts with tap water even in an emergency! Well water and even some city water may have microbes and parasites you do not want in your eyes.
5. How to properly insert a contact lens (step-by-step)
To insert:
- Wash and dry your hands on a clean towel.
- Remove the contact from its case with your thumb and index finger and place it on the index finger.
- If the contact is not a bowl shape, turn it the other way.
- Use your other hand to slowly lift your eyelid.
- Look up and slowly place the lens on the eye, giving it 1 second to suction to your eye fluids.
- Once you feel it attached, blink slowly to strengthen its bond in the right position.
- Dump any solution left in your case into the sink and allow the case to dry completely. A CDC study found that as many as 55 percent of contact wearers don’t use new solution every time, which is scary given the number of dangerous eye infections you can contract with poor contact hygiene.
To remove:
- Wash your hands.
- Prepare your case with new solution.
- Pull your eyelid up with one hand.
- Look up.
- Gently slide the contact onto the white of your eye.
- Grab the contact with a thumb and index finger.
- Place the contact carefully in the case and close the case.
6. How to stop dropping the contact during insertion or removal
Be patient with yourself. The main reason people struggle is they see how quickly others can insert and remove contacts, but the people who do it quickly have been wearing contacts for at least a couple of weeks. Give yourself a little extra time in the morning to get the hang of it, and soon, you’ll be as fast and flawless as they are.